Genome editing is a powerful tool that enables precise changes in the genetic code of a cell. Genome-edited hematopoietic stem and progenitor cells (HSPCs) yield genome-corrected cells of all lineages, yet the only cell type of clinical relevance in red blood cell (RBC) disorders is the RBC. Most applications of genome editing have sought to correct disease-causing mutations of monogenic diseases. However, human genetic variation reveals variants that confer positive health benefits as well. In this study we took advantage of a naturally occurring human variant to increase erythropoietic output from genome-edited HSPCs. The variant leads to a condition termed congenital erythrocytosis (CE), a rare phenotype in which people have higher than normal levels of RBCs and consequently elevated hemoglobin. It is caused by truncations in the erythropoietin receptor (tEPOR) in which the intracellular inhibitory domain to erythropoietin (EPO) signaling is eliminated. The genetic cause of this phenotype was identified in a family of a Finnish Olympic gold medal-winning cross-country skier who was found to have levels of hemoglobin >50% higher than normal. One of the challenges in gene therapy is to achieve sufficient engraftment of genetically engineered cells to have a clinical effect. Here we sought to give edited cells a selective advantage such that low levels of engraftment might still result in a clinical benefit through use of genome editing to recreate the CE phenotype by engineering tEPOR into HSPCs in different ways.
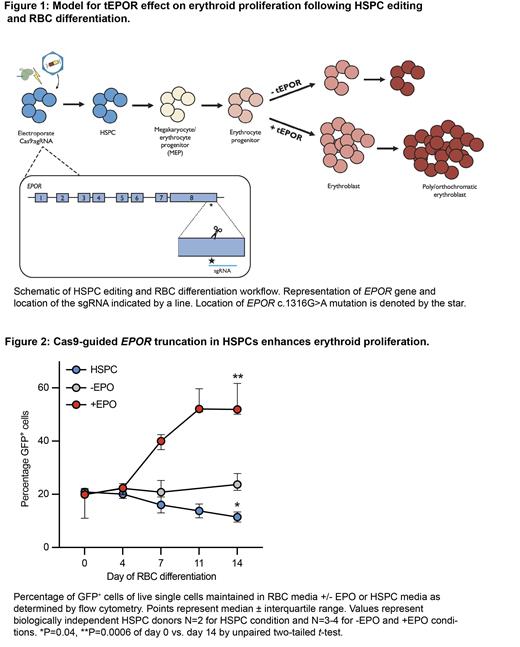
We hypothesized we could recapitulate the CE variant using CRISPR/Cas9 genome editing of HSPCs to create insertions/deletions (indels) at the EPOR locus near the site of the mutation ( EPOR c.1316G>A) and then transfer the cells into culture media that promotes erythroid differentiation (Fig. 1). We demonstrated increased erythropoietic output from cells containing truncating mutations in EPOR, measured by an increase in indel formation throughout erythroid differentiation (1.3-3.8-fold increase). Because not all indels created cause truncations in EPOR, we explored if we could amplify this effect by integrating an AAV6 repair template that introduces a stop codon into EPOR followed by a BGH-polyA tail and GFP marker driven by a constitutive UbC promoter. This strategy enriched for GFP + cells with the truncation even more dramatically as they developed during erythroid differentiation (2.5-4.6-fold increase). We also found a substantial increase in the total number of cells produced from the tEPOR edited condition at the end of differentiation (3.3 times greater fold increase compared to mock edited cells). Importantly, we observed no enrichment in cells kept in HSPC media or cultured in RBC media without EPO, indicating this effect is EPO-dependent (Fig. 2). Next, we investigated whether a tEPOR cDNA could be targeted to the CCR5 safe harbor locus under ubiquitous expression or to the HBA1 RBC-specific safe harbor site imparting high levels of erythroid specific expression. Integration of the tEPOR cDNA at both loci yielded strong enrichment of edited alleles in an EPO-dependent manner when put through erythroid differentiation (6.2-8.6-fold increase at CCR5 and 2.9-5.2 at HBA1). Lastly, we sought to pair the tEPOR cDNA with a clinical edit for β-thalassemia to boost production of disease-corrected RBCs. We showed that through use of bi-cistronic cassettes we were able to drive a >2-fold enrichment of edited alleles over the course of differentiation. Additionally, we were able to pair the tEPOR cDNA and clinical edit for β-thalassemia through multiplexed gene editing at EPOR and HBA1, respectively, and again demonstrated enrichment of edited alleles.
Ultimately, we believe this work has the potential to amplify the efficacy of gene and cell therapies for blood disorders currently in the clinic. Expression of tEPOR could be integrated into any treatment for blood disorders that involve transplantation of HSPCs, including both allogeneic and autologous bone marrow transplants. Further, as low chimerism in the bone marrow could produce high levels of peripheral RBCs using our strategy, it has the potential to reduce the morbidity of myeloablation regimens currently required for cure of blood disorders. This work, in effect, has the potential to improve the safety and accessibility to currently available treatments for the millions of patients affected by RBC disorders worldwide.
Disclosures
Sheehan:Beam Therapeutics: Research Funding; Refoxy Pharmaceuticals: Research Funding; Afimmune: Research Funding; Pfizer Inc: Research Funding; Novartis: Research Funding. Porteus:Graphite Biologics: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees; Allogene Therapeutics: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees; Alaunos Therapeutics: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees; Kamau Therapeutics: Current equity holder in private company; CRISPR Tx: Current equity holder in publicly-traded company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal